
In this blog, we hear from Risk Analyst Catherine McCarthy as she talks about an opportunity APHA had to produce a risk assessment for human international air travel … something very different for us!
On the June 1 2020, on what was the 70th day of a long and arduous lockdown, I, alongside colleagues from the Animal and Plant Health Agency (Rachel Taylor, Virag Patel, Ruth Moir, Louise Kelly and Emma Snary), had a meeting with Public Health England’s (PHE) modelling team.
As coronavirus case numbers in the UK had started to come down, policy makers were beginning to talk about resuming international travel (all non-essential travel had been advised against since the 17 March).
The PHE modelling team correctly predicted that this would be a future topic that would require scientific advice to inform UK Government policy, and asked if we would be able to produce a risk assessment for international air travel. Keen to help our public health colleagues, we agreed. We regularly produce import risk assessments for a range of zoonotic and animal diseases, however this brought us some new challenges.
Not only was this work going to influence UK government policy and so needed to meet our usual quality standards, but we also needed to finish the whole project (including understanding all the risks involved in international travel, gathering the data, writing the computer code for the model, producing the results, checking the accuracy of the results and writing a report) within three and a half weeks.
Action stations!
The first task was to get our head around the fact that this was a human disease. Yes, we were used to producing risk assessments and working with complicated datasets, but there are differences in modelling a human instead of an animal disease.
For a start, if an exotic disease emerges on a farm then we can request that farmers stop animals from leaving the farm. Turns out that people are less keen to hear that they need to stay in self-isolation for 14 days after their summer holiday, and some people don’t follow the advice.
Modelling human behaviour is certainly an extra challenge!
In the end, we had decided on our framework: we considered the risks that a UK citizen would be infectious before they went on a trip abroad, or that a UK citizen would catch coronavirus during their trip and bring it back to the UK, or non-UK citizens travelling to the UK would be infectious and bring the disease into the UK.
International travel risks
We looked at several key factors in order to understand which countries pose the greatest risk to the UK.
Firstly, we wanted an accurate understanding of how many cases were in each country. Although this sounds fairly simple (after all, the number of positive cases are reported each day from every country), these numbers are only the tip of the iceberg because they only report known positive cases. If someone has not had a test then they will not be detected. This could either be because there are not enough tests available to test everyone (test availability varies widely between countries), or because someone has not developed (sufficient) symptoms to ask for a test (the so called asymptomatic cases).
This team, led by Virag Patel, developed a new method for accurately calculating the number of cases in each country (the preprint is now available). This work is currently being used to provide a weekly update to PHE and the UK Overseas Territories on the number of cases in each country.
However, understanding the risks from international travel was even more complicated. We also needed to incorporate the number of flights from each country and the probability that travellers will be infected whilst on their trip. Therefore we developed a sophisticated computer program which enabled us to rank countries by the risk of bringing SARS-CoV-2 (the virus responsible for coronavirus disease) into the UK.
Part of the difficulty was how rapidly the disease was changing in Europe. Out of the countries that we were looking at, the ranking of most risky countries became outdated every week.

We knew that the UK government were planning on asking people from high-risk countries to isolate for 14 days upon arrival to the UK. We were asked by PHE to see whether we could identify alternative strategies which would not require such a long self-isolation.
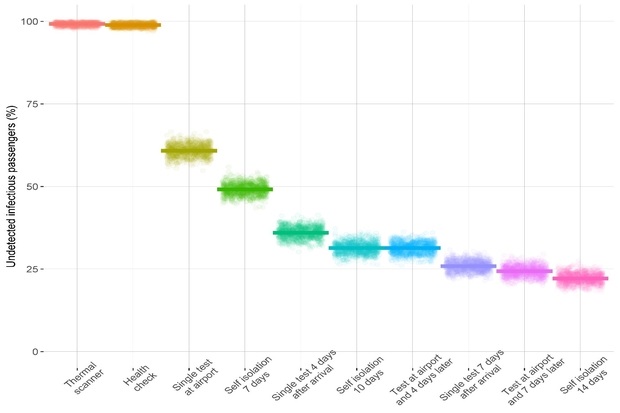
Thermal imaging scanners (which detect if someone has a fever) and health checks have been used in previous epidemics (like the Ebola epidemic in 2014-2016). Testing for the virus has been suggested by many airport representatives as an alternative to the self-isolation. Question is, were they effective? Actually our work showed that they all have a very low detection rate. For example, if airports relied on thermal imaging scanners as their only detection method then they would only identify one in every 128 infectious passengers.
Virus testing was slightly better, but would still only detect two in five infectious passengers. We found that the test accuracy could be improved if the samples were taken four days after a passenger has arrived in the UK. Ultimately though, nothing was found to be as effective as quarantine for 14 days. Please see our preprint, ahead of a scientific publication.
What did we learn about providing advice for public health policy makers?
Not only did our results constantly need updating due to the ongoing pandemic, our objectives also kept expanding. Additional policy requests meant that we had to expand the health measures that we looked at as well as producing an interim report for PHE one weekend mid-way through the project.
By the June 24, we finished our 62 page risk assessment report (led by Rachel Taylor and myself) for PHE. It was sent to the Scientific Pandemic Influenza Group on Modelling (SPI-M) meeting on the following day and has since been shared and/or used within the Chief Scientists Office, Department of Health and Social Care, Home Office, Cabinet Office, Joint Biosecurity Centre and the Scottish Government. The risk assessment was also used to aid decisions by the Ministry of Justice on the risk of introducing SARS-CoV-2 through infected prisoners entering prisons.
It is exciting to think that we have made a tangible impact helping with the coronavirus pandemic. The pressure to be accurate but to deliver at pace were high and only possible through a combined team effort.
Although coronavirus is a zoonotic disease, by far the majority of transmission is human-human. As an animal infectious disease modeller, it was insightful to work on a disease directly spread between humans. I hope we can call on our public health modellers during our next major animal disease outbreak.
Find out more
You may be interested to read some of our previous blogs from the Department of Epidemiological Sciences:
Department of Epidemiological Sciences: Expertise with impact!
Global thinking: Modelling pathogen risk and spread across borders
Modelling: the next generation
Enjoyed reading? Then why not subscribe to the APHA Science Blog
Recent Comments